The COVID-19 pandemic has had a sweeping impact on individuals, businesses, and industries throughout the world, but few sectors have felt as pressing a strain on resources as health care.
As first responders and other providers helm the front lines of the coronavirus outbreak, medical professionals across all fields are paying close attention to regulatory shake-ups that affect how they practice and care for patients.
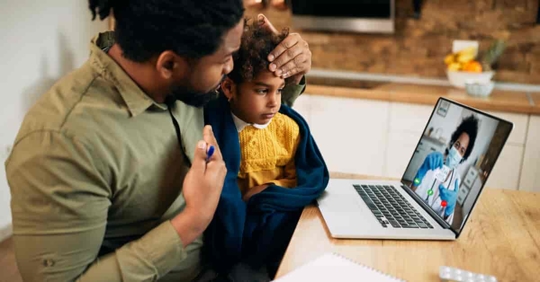
Chief among them: revised rules for telemedicine.
Federal Regulators Loosen Telehealth Rules to Curb Coronavirus
In a series of unprecedented emergency response efforts, the federal government has turned to telehealth services to reduce strains on our health care system and mitigate the spread of COVID-19.
Under the Coronavirus Preparedness and Response Supplemental Appropriations Act, the CARES Act, and various emergency orders, a number of regulatory flexibilities and policy changes are now in effect:
- For the duration of the national emergency, Medicare will pay for Medicare telehealth services provided to beneficiaries in all parts of the country and in all settings at the same rate as regular, in-person visits. Prior to this waiver, Medicare could only pay for telehealth for persons on a limited basis: when the person receiving the service is in a designated rural area and when they leave their home and go to a clinic, hospital, or certain other types of medical facilities for the telehealth service.
- CMS expanded the types of health care professionals that can provide telehealth services to include all those eligible to bill Medicare for professional services. As a result, a broader range of health care professionals, such as physical therapists, occupational therapists, speech language pathologists, registered dietitians, nutrition professionals and clinical psychologists, can use telehealth to provide services to Medicare beneficiaries. These visits are considered the same as in-person visits and are paid at the same rate as regular, in-person visits. This waiver went into effect retroactively on March 1, 2020 and will continue through the end of the emergency declaration.
- CMS has allowed practitioners to provide certain services via audio-only equipment by waiving requirements that technology platforms must allow for two-way video interaction. A complete list of Medicare telehealth services that meet the requirements for audio-only interaction can be found here. The effective date of this waiver is March 1, 2020; it will continue through the end of the emergency declaration.
- The Department of Health and Human Services (HHS) has also taken steps to make it easier to provide telehealth services. The HHS Office of Inspector General (OIG) is providing flexibility for providers to reduce or waive cost-sharing requirements for telehealth visits paid by federal health care programs, such as Medicare, Medicaid and the Children’s Health Insurance Program (CHIP). This statement was issued March 17, 2020 and will continue throughout the public health emergency.
- The HHS Office for Civil Rights increased HIPAA flexibility during the COVID-19 public health emergency, and will not penalize physicians for non-compliance when they serve patients in good faith via common communication technologies such as Skype or FaceTime, even if the application does not fully comply with HIPAA rules. However, providers should not use any platforms that are public-facing — such as Facebook Live, Twitch or TikTok — to provide telehealth.
- The Drug Enforcement Administration (DEA) has adopted policies to allow registered practitioners to prescribe controlled substances without having to interact in-person with patients. Federal law still requires prescribing practitioners to use sound judgment to determine if the issuance of prescriptions is for a bona fide medical purpose, and for providers to also comply with applicable state law. A decision tree published by the DEA summarizes the new prescribing policies. These policies became effective beginning March 31, 2020 and will remain in effect for the duration of the public health emergency.
State Medical Boards Alter Telemedicine & Licensing Policies for COVID-19
In addition to policy changes at the federal level, many states have lifted restrictions requiring health care providers to be licensed in the state where a patient is located at the time of treatment, as well as regulations related to retired or clinically inactive physicians.
The Federation of State Medical Boards (FSMB) COVID-19 webpage details the latest regulatory updates and resources regarding state emergency declarations and licensing waivers, which are constantly evolving.
In Texas, for example:
- Governor Greg Abbot directed the Texas Medical Board (TMB) and Texas Board of Nursing (TBN) to fast-track temporary licensing of out-of-state physicians, PAs, certain retired physicians, nurses, and other licensed providers.
- The TMB will automatically extend license and permit expiration dates. Permits for licensees which expire on 2/28/2020 or 5/31/2020 will be extended through 8/31/2020, and late fees will be waived. Continuing Education requirements related to renewal extension will also be waived.
Texas Medical Board Telehealth Policies During COVID-19
In addition to waiving certain licensing requirements, states like Texas are also promoting the expansion of telehealth services. Per the TMB and TMB COVID-19 FAQ:
- Texas Occupation Code 111.005 (a)-(b) and Title 22, Chapter 174.6 (a)(2)-(3) of the Texas Administrative Code are temporarily suspended until terminated by the Office of the Governor, or until the disaster declaration is lifted. As a result, telemedicine, including the use of telephone only, may be used to establish a physician-patient relationship and for the diagnosis, treatment, ordering of tests, and prescribing for all conditions. The standard of care must be met in all instances, and TMB emphasizes the need to properly document a telemedicine visit.
- Also as a result of the emergency rule, doctors will be eligible for payment from insurance plans regulated by the Texas Department of Insurance (TDI) for medical visits they conduct over the phone at the same rate for telemedicine services as for in-person services, including covered mental health services.
- TMB has extended a waiver of Title 22, Chapter 174.5 (e)(2)(A) of the Texas Administrative Code. The waiver allows telephone refills of a valid prescription for treatment of chronic pain with an established chronic pain patient. Due the seriousness of the opioid crisis, the waiver was initially only in effect until April 10, 2020, but was extended until September 2, 2020 or for the duration of the disaster declaration. This waiver follows the DEA announcement, referenced above, that health care professionals can prescribe controlled substances, including opioids, via telemedicine during the current public health emergency.
Hendershot Cowart P.C.: Trusted, Knowledgeable Counsel for Health Care Providers
Amid many ongoing developments in the coordinated response to COVID-19, health care providers who are now eligible to provide telehealth services face an onerous task of ensuring adherence to complex regulatory and coverage requirements prior to submitting claims for reimbursement.
At Hendershot Cowart P.C., our health and medical law team is actively counseling health care providers across Texas and the U.S. in a range of matters arising from the coronavirus outbreak. That includes eligibility evaluations, Medicare matters, and complex telemedicine rules and guidelines for coding, telehealth compliance, billing for services, reimbursement, technology, and regulatory compliance. Contact us to speak with an attorney.